#explainer
So You’re Thinking About Getting an IUD
health
·5 min read
by Toni Brannagan | 11/18/2020
If you’re exploring a long term birth control option, and the pill just ain’t cutting it anymore, one of the choices your gynecologist may recommend an IUD, or intrauterine device. An intrauterine device is pretty self-explanatory — it’s placed inside your uterus (quick anatomy lesson: that’s past your vagina and cervix, so it’s not just floating around in your V like a tampon.)
IUDs are pretty much the equivalent of a celebrity’s rise to fame being an *overnight success*. It might seem like everybody just started talking about them all the time out of nowhere, but IUDs have actually been chugging along as a birth control option since 1909! (TL;DR — the first IUDs were made out of silkworms.) A century later, Guttmacher Institute reports that just 12% of women who use contraception have an IUD, which follows an increasing growth pattern from 2% in 2002, 6% in 2007, and 9% in 2009. As IUD-usage becomes more widely recommended as a safe and reliable long term form of birth control, especially while more low-hormone options are popularized (more details on that later!), those numbers are bound to grow even more.
Here’s the thing: Birth control is a super personal choice, since what works and what doesn’t work is often so different for everybody. That’s especially the case with IUDs — a few factors to consider with your doctor are whether it’s covered by health insurance, whether an IUD insertion (and removal!) is right for you, and maybe most important, how your body reacts to the IUD. When it comes to our bodies, choices are hardly ever one-size-fits-all, so keep that in mind, too!
So what’s so great (and not-so-great) about having an IUD?
the pros of having an IUD
As you may already know, an IUD is a popular choice for folks who are looking for longterm contraception that’s pretty low maintenance. *Set it and forget it*, if you will. After an IUD is inserted by your gynecologist, a process that some folks describe as a pinch and others describe as indescribable searing pain (others may be me), they will usually follow up a few months later to make sure everything’s still in place. Typically, that’s it.
Also, while FDA-approved IUDs vary between 3 years and 12 (!) years of effectiveness, you’re also not obligated to keep an IUD the entire time. Sick of it after 2 or 3 years? It can be easily removed, and has no long term effects on fertility.
what’s the catch?
First things first: IUDs are obviously not a barrier method, and do not protect from STIs like condoms do. This may make an IUD on its own an unsuitable option for people who have multiple partners, or are at risk of contracting STIs from their partner. There is also a risk of infection that comes with getting an IUD, which is highest during insertion.
If you use contraception with the goal to prevent pregnancy, it’s also worth noting that no method is perfect, and even if an IUD is over 99% effective, that .01% still exists. Getting pregnant with an IUD can also lead to an ectopic pregnancy, an infection, or other complications — if you suspect you’re pregnant and have an IUD inserted, you should see a doctor immediately.
IUDs also aren’t recommended for people who have an STI themselves, have uterine or cervical cancer, and may be pregnant (you will typically be given a pregnancy test before insertion to double-check). Having a convo with your gynecologist about potential risks first is a must!
Like every other form of birth control, the side effects one may experience with an IUD will also probably make or break whether it’s a method for you. These vary between hormonal non-hormonal IUDs, so let’s break it down further:
mirena and kyleena and liletta, oh my!
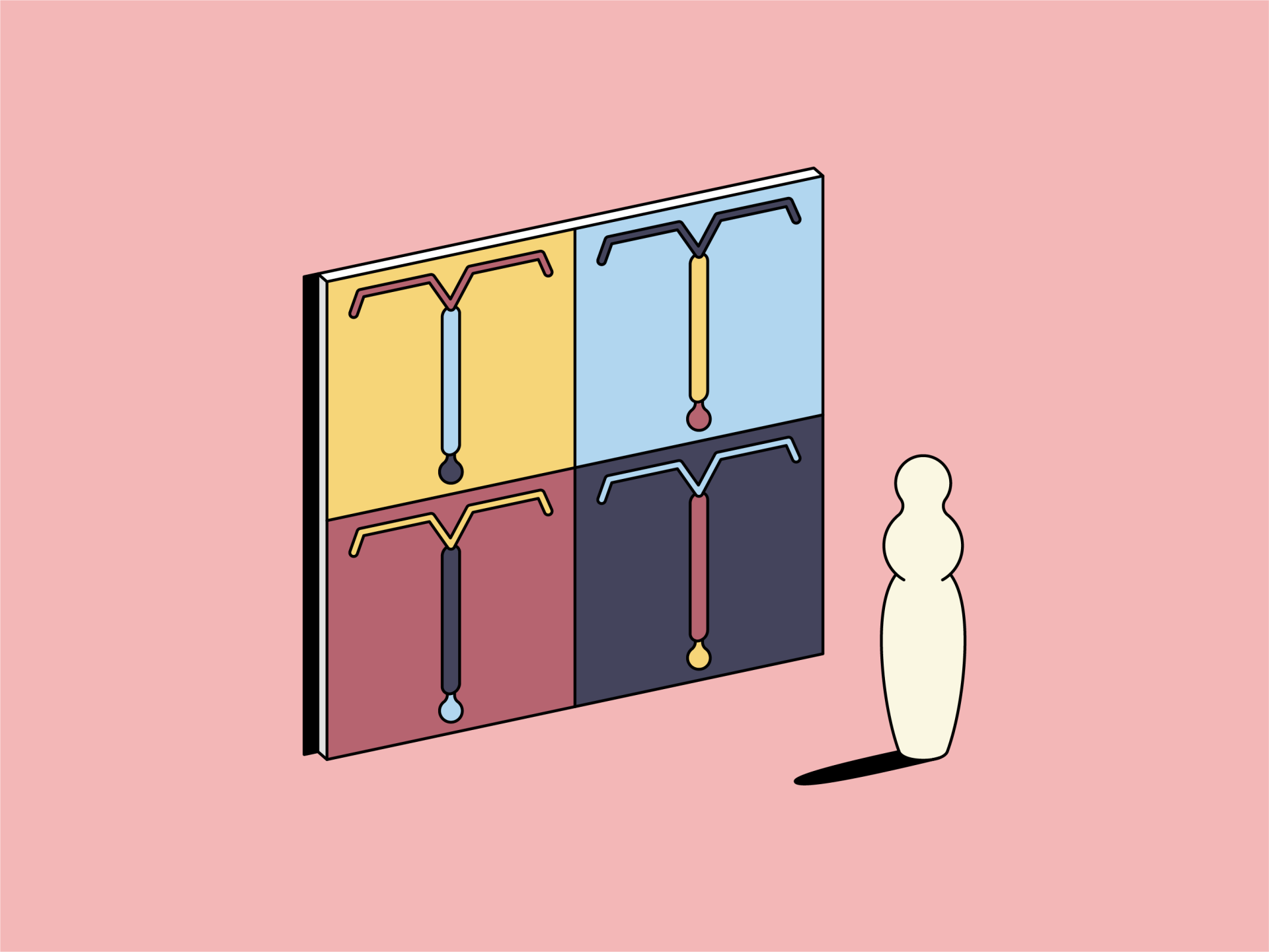
There are four FDA-approved hormonal IUDs: Mirena, Kyleena, Liletta, and Skyla. They vary in size, and hormone dose. You can check out a more detailed breakdown of all of these guys, including experiences from people who have used them (+ mine... pro-tip: stock up on Thinx for post-insertion spotting) right here.
A hormonal IUD does its job by making it much, much harder for your eggs to be fertilized. They release the hormone levonorgestrel, which can prevent ovulation entirely, thicken your cervical mucus to prevent sperm from getting close to an egg, and keep your uterine lining from thickening. This is why a hormonal IUD can sometimes make your periods go away entirely — at the least, they will get much lighter depending on your usual flow.
Besides preventing pregnancy, these effects can be prescribed to help people with endometriosis, period pain, anemia, fibroids, and more. On the flipside, hormonal IUDs aren’t recommended for people with breast cancer, liver disease, or pelvic infections, and may not be suitable for people with migraines, high blood pressure, or certain prescriptions.
the natural option
If you like to keep your hormones and your BC separate, the copper IUD Paragard could be the one for you. As the name suggests, the copper IUD uses copper to ward off sperm, which is pretty metal (haha… get it?). Copper is basically sperm kryptonite — it makes them swim weird and lose their sense of direction, so they can’t find the egg to fertilize. It’s pretty cool.
For many people, the allure of the copper IUD is that it’s a natural, hormone-free birth control option. Paragard is approved for use up to 12 years, making it the most longterm option if it’s right for you. Some factors to consider are that your periods may get heavier and crampier, especially in the first 6 months — if your natural periods are already heavy and crampy, it might not work out.
If you’re interested in getting an IUD, make an appointment with your gynecologist to figure out if it’s a good option for you, and which one makes the best fit.
Have you ever had an IUD? Are you considering getting one? Share your comments and concerns with us below!
Toni Brannagan is a writer and was the former Copy and Content Manager at Thinx.
by Toni Brannagan